Predicting Seizures in Epilepsy Patients
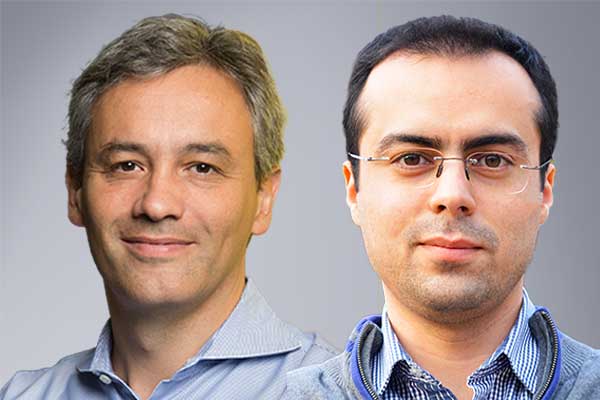
ECE Professor Tommaso Melodia and Principal Research Scientist Pedram Johari, in collaboration with Joseph Neimat from the University of Louisville, Jorge Jimenez from the Georgia Institute of Technology, and Doug Pham from Microchip Technology Inc., received a $550K NSF Partnerships for Innovation – Research Partnerships (PFI-RP) grant for “Smart Seizure Prediction System based on AI-enabled Implantable Sensor Networks.”
The SeizNet team includes strong subject-matter expertise in intra-body ultrasonic communications, embedded AI systems, IoT (Institute for the Wireless Internet of Things at Northeastern University); expertise in medical device development, signal processing, and biosensor design and testing (Biomedical Engineering Department at Georgia Institute of Technology); clinical expertise from a leading neurosurgeon specialized in movement disorders including epilepsy (Department of Neurological Surgery of the University of Louisville); expertise in low-power computational hardware (FPGA Business Unit at Microchip Technology Inc.).
This PFI-RP project has a strong potential for societal impact, specifically in providing a better quality of life for patients affected by epilepsy. The technology to be developed as part of this PFI partnership has a number of additional medical applications, including cardiac pacemakers and in stimulation for Parkinson’s disease or PTSD patients. The project will train Ph.D. students with a strong focus on hands-on, interdisciplinary work with a significant entrepreneurial component and opportunities to interact with established professionals in the field.
Abstract Source: NSF
The broader impact/commercial potential of this Partnerships for Innovation – Research Partnerships (PFI-RP) project is to provide a better quality life for patients affected by neurological disorders for whom antiepilepsy drugs are not effective. While the technology will focus on novel treatments for drug-resistant epilepsy, a number of additional medical applications, including the treatment of patients with cardiac pacemakers, Parkinson disease, or post-traumatic stress disorder (PTSD) could be possible. According to the Centers for Disease Control (CDC), 1.2% of the US population (about 3.4 million people) has active epilepsy with more than 65 million people affected globally. While epilepsy patients have benefited from Implantable Medical Devices (IMDs), none of the current Food and Drug Administration (FDA)-approved neurostimulators that are used to alleviate seizure intensity in patients with drug-resistant epilepsy offer preventive treatment or well-in-advance, accurate, predictive alerts. This project may enable medical professionals to accurately predict a seizure so that patients could take precautions and avoid adverse outcomes such as serious injuries or death.
The proposed project will enable in-situ smart medical inference via embedded Artificial Intelligence (AI) algorithms for patients affected by neurological disorders not treatable with antiepilepsy madications. The treatment may eliminate the need for subcutaneous wiring and highspeed through-body wireless links, offering a safer and more energy efficient solution. Currently, commercial neurostimulator systems use wired leads from a subcutaneous generator to send electrical signals to the targeted stimulation site. This wiring is a major cause of post-operative complications. Additionally, most of these systems are open-loop and have limited edge-computing capabilities. They require significant manual clinician input to adjust their response parameters and some still use continuous stimulation since they cannot predict a seizure. This project may improve deep brain and other neurostimulation technologies by developing intelligent and wirelessly-powered implants with embedded, in-situ, AI processing. This development may remove the dependency of the prediction models on external cloud computing, which requires transmission of a steady stream of data from implantable sensors to external devices. Wireless connectivity, re-chargeability, and re-programmability will be added to the system through low-power ultrasonic waves. This innovation may eliminate the needs for subcutaneous wiring between electrodes and implants and for large, implanted batteries.